The Ethics of Retail Radiology
Hey everyone, I'm currently between graduation and residency, so I've decided to post an essay I wrote for one of the last courses of medical school: Medical Ethics. The essay focuses on a controversial topic in my chosen field, radiology. Enjoy!

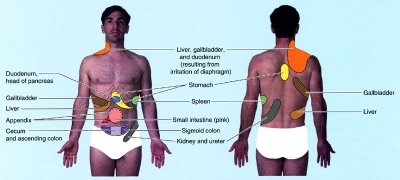
Image source:
The Ethics of Retail Radiology
Imagine a future where diseases are caught in their infancy and disorders are slowed, stopped and even reversed before patients ever suffer from the symptoms. With AccuScan, that future is available right now, right here in Salt Lake City (1).
Nestled between a megaplex and a boutique in the Gateway outdoor mall, AccuScan Health Imaging is a body imaging center that offers the promise of early disease detection in asymptomatic individuals. No physician referral is required; any customer willing to pay out-of-pocket can choose from a selection of computed tomography (CT) screening exams, including whole body scan, heart scan (coronary artery calcium screen), lung scan, head scan, and virtual colonoscopy. The scans are read by a board-certified radiologist and the patient receives the images, a detailed written report, and referral to a specialist if there are any concerning findings (1).
A decade ago, self-referred body imaging centers were on the rise, fueled by publicity on talk shows, stories in health magazines, direct-to-consumer (DTC) advertising, and dissatisfaction with managed care. Within a few years, however, the retail radiology bubble burst, and many initially successful centers went out of business (2). The collapse has been attributed to economic forces (e.g., competition driving down prices) and the influence of medical professional societies, which have been uniformly skeptical of the value of whole-body screening. Critics have raised many concerns, such as unethical advertising, unnecessary radiation exposure, high false-positive rates, and low cost-effectiveness (3-6). The FDA warns that "whole-body CT screening has not been demonstrated to meet generally accepted criteria for an effective screening procedure" (7).
In spite of these misgivings, the demand for imaging centers like AccuScan has not evaporated completely. They remain unregulated by the FDA (7). A recent survey found that 2% of radiologists still support whole-body CT screening, and many more support CT screening exams of the heart or lungs in particular patients (3). Supporters emphasize the patient’s right to know and argue that the benefits of early disease detection outweigh the risks (8,9).
Are self-referred imaging centers ethical? In this paper I would like to examine the controversy in the light of widely accepted bioethical principles: autonomy, beneficence, nonmaleficence, and justice. How does each principle support or discredit the practices of retail radiology? At the end, rather than simply applying the label of "ethical" or "unethical," I would like to address a more practical question: what can businesses like AccuScan do to function as ethically as possible?
Autonomy
Take control of your own health and stay as healthy as you feel with AccuScan (1).
One of the most compelling arguments in favor of self-referred imaging centers is patient autonomy. Proponents view their services as a form of "medical self-empowerment" (9). Frustrated with a "paternalistic payor-physician culture that controls the practice of medicine and patient referral,"(10) some customers are willing to pay more for a different kind of experience. In addition to data the patient cannot obtain from their regular providers, AccuScan promises a visit with "no green scrubs, sterile surroundings, long waits, or impersonal treatment" (1). Patients enjoy the highest possible sense of autonomy because they are paying out-of-pocket for a service of their choice.
However, critics contend that patients are choosing whole-body CT scans with incomplete or even inaccurate information (6). According to the AMA Code of Ethics, the "patient’s right of self-decision can be effectively exercised only if the patient possesses enough information to enable an informed choice" (11). One analysis of print advertisements and brochures concluded that DTC marketing of self-referred imaging services "fails to provide prospective consumers with comprehensive balanced information vital to informed autonomous decision making" (5). For example, there was typically no information on the rate of false-positive findings and the procedures needed to evaluate indeterminate lesions. Many ads conveyed a false sense of reassurance, some evoked fear (5).
Beneficence
Many diseases progress silently, leaving you totally asymptomatic... AccuScan can provide early detection, allowing physicians to slow, stop, or in some cases reverse disease long before your symptoms would have led you to seek help (1).
Most consumers who seek whole-body CT scans and other screening exams are motivated by the benefits of early detection. Indeed, early detection leading to treatment and improved survival rates is the rationale for mammography, colonoscopy, and other scientifically validated screening exams. If screening for disease in selected organs is good, why not go for the whole body? A whole-body CT scan is a rapid (15 minutes), painless, noninvasive method of acquiring an extraordinarily detailed picture of internal anatomy. One radiologist, Richard Penfil, expressed the sentiment this way:
Historically, you go to your internist once a year and he thumps on your chest, takes out his stethoscope, draws some blood to send to a laboratory, sends you for a chest x-ray, and asks how your golf game is doing. That, to me, is the virtual examination. The actual examination is where you take a look at what is going on inside your body (12).
From a scientific perspective, however, the effectiveness of whole-body CT as a screening exam is unproven (7,13). Although anecdotal evidence makes the headlines (8), there is "no evidence that total body CT screening is cost efficient or effective in prolonging life" (13). The potential benefit of early detection may be outweighed by adverse effects and wasteful costs (discussed below).
On the other hand, no randomized controlled trial (RCT) - the gold standard for evidence-based medicine - has been designed to study screening with whole-body CT. Supporters argue that the "delay imposed by a randomized clinical trial (perhaps a decade) makes such a trial's results an unacceptable Holy Grail" (9). Other CT screening exams are growing in scientific support as evidence accumulates, at least in certain patient populations (3). Initially controversial, coronary artery calcium screening is now recommended for patients at moderate risk for heart disease (14). CT lung screening in smokers is still intensely debated, but a large RCT - the National Lung Screening Trial - should clarify things (15). CT colonography (virtual colonoscopy) is widely considered an acceptable option for colorectal cancer screening (16). Given the possibly life-saving benefits of a whole-body CT, why should we have to wait for stronger evidence?
Nonmaleficence
Our protocols are built to insure the lowest dose possible, minimizing risk to non-calculable levels. The breast tissue in the chest CT study is exposed to no more radiation than a mammogram (1).
Perhaps the most common ethical dilemmas in clinical medicine involve the balance of beneficence and nonmaleficence, or potential benefit vs. potential harm. Critics claim that the potential benefits of whole-body CT screening exams are exaggerated and the risks are minimized or not discussed at all.
To be embraced by the medical community, screening exams must meet certain criteria. For example, the exam should be good at detecting disease that is both serious and treatable if caught early. Effective screening programs minimize false positives and false negatives and maximize cost effectiveness by focusing on populations in which there is a higher prevalence of the disease. CT colonography, for example, is usually recommended only for patients 50 years or older (16).
Whether whole-body CT could ever meet the criteria of an effective screening program is unknown, but preliminary data are not encouraging. One study based on a hypothetical cohort of 500,000 asymptomatic 50-year-old men found that whole-body CT scans are more expensive, in costs per life-year, than most health care interventions currently funded in United States (4). One serious concern is the high rate of false positives in populations with a low prevalence of disease. In a recent study of patients seen at one outpatient imaging center in California during a 6-month period, 86% of the 1192 patients (mean age 54 year old, most self-referred) had at least one abnormal finding described in the whole-body screening report (17). In many cases there are no standard criteria for deciding which lesions need further work up. Many findings that do require further evaluation - such as certain renal masses - are likely to be indolent diseases that never would have bothered the patient if they had not been discovered on CT (18).
Additional work up means additional anxiety and risk for the patient. In the California study, 37% of patients received at least one recommendation for further evaluation, most commonly additional imaging of lungs or kidneys with intravenous contrast (17). Indeterminate findings could also lead to invasive procedures such as biopsy, surgery, or endoscopy; however, none of these were specifically recommended in the California study (17).
What about the radiation risk from CT exams? Although the degree of risk has been debated, it appears to be small. One study estimated that the radiation dose from a single whole-body CT screening exam is approximately 15-20 mSv (millisieverts). For a 45-year-old adult receiving a single exam, this dose increases the risk of death from cancer by 0.08% (19). AccuScan claims the dose of its whole-body CT screen is 5.2 mSv, or 1/2 to 1/3 the dose of conventional CT study (1). This dose is comparable to the natural background radiation exposure to the average American in one year (3.1 mSv).
Justice
AccuScan is another tool in the arsenal against disease. It is meant to supplement and enhance traditional health care, not replace it (1).
In bioethics, distributive justice refers primarily to the equitable use of limited health care resources. For critics of retail radiology, the main concern here is the additional demand for medical resources created by false positives and the discovery of indolent disease (17). Consumers pay out-of-pocket for the initial scan, then funnel into the traditional health care system for follow up if recommended. Some physicians may find themselves in the awkward position of having to provide education and management based on a scan they did not order or discuss with the patient before it was performed (6).
Recommendations
In any medical setting, some activities - using fear in advertising, making false promises, failing to provide informed consent - are clearly unethical. Other activities, such as selling CT screening exams directly to the public, are more ethically ambiguous. Precisely where the activities of self-referred imaging centers fall on the ethical continuum depends partly on which principles are most heavily weighted. Proponents tend to emphasize autonomy and beneficence; detractors tend to emphasize nonmaleficence and justice. Here are some recommendations for making the practice of retail radiology as ethical as possible.
- Perhaps most importantly, providers of any screening exam must obtain true informed consent (20). Patients do have a right to make decisions about their own health care, even if the physician does not agree with the decision. However, respect for autonomy does not mean the patient should make health care decisions in a vacuum. An important responsibility of the physician is to create the conditions for a truly informed choice about procedures and tests, making sure the patient understands the benefits, risks, and limitations. Patients are often aware of a small radiation risk, but are less likely to understand the risks of false positives and the potentially invasive and costly work up and treatment of indolent disease. Patients should be warned against a false sense of security that comes with a negative exam.
- Advertisements should be free of unsubstantiated scientific claims, exaggerated promises, or scare tactics. If abuses continue, DTC marketing of imaging services should be subjected to regulatory control similar to what currently exists for the pharmaceutical industry (7).
- Providers should be wary of screening everyone who walks in the door. Patients should be informed of the evidence-based guidelines, if any, for the screening exams they would like to receive. Of course, a challenge for all medical entrepreneurs is putting the patient's welfare ahead of financial interests. According to an early advocate of CT screening, "most centers attempt to exclude individuals who are younger than 40 years old, but the financial incentive clearly tempts some to lower the threshold" (9).
References
- AccuScan Health Imaging. Available at http://www.accuscanhealthimaging.com/
- Kolata G. Rapid rise and fall for body-scanning clinics. New York Times, 23 Jan 2005. Available at http://www.nytimes.com/
- Burger IM, Kass NE, Sunshine JH, Siegelman SS. The use of CT for screening: A national survey of radiologists' activities and attitudes. Radiology 2008; 248:160-168.
- Beinfeld MT, Wittenberg E, Gazelle GS. Cost-effectiveness of whole-body CT screening. Radiology 2005; 234:415-422.
- Illes J, Kann D, Karetsky K, et al. Advertising, patient decision making, and self-referral for computed tomographic and magnetic resonance imaging. Arch Intern Med 2004; 164:2415-2419.
- O'Malley PG, Taylor AJ. Unregulated direct-to-consumer marketing and self-referral for screening imaging services. Arch Intern Med 2004; 164:2406-2408.
- FDA. Whole-body CT screening - should I or shouldn't I get one? Available at http://www.fda.gov/
- Nii JK. A new image. Deseret News, 30 Aug 2004. Available at http://www.deseretnews.com/
- Brant-Zawadski M. CT screening: Why I do it. Am J Roentgenol 2002; 179:319-326.
- Barnes E. Whole-body CT: Radiology to the people. AuntMinnie.com, 2 Oct 2002. Available at http://www.auntminnie.com/
- AMA Code of Medical Ethics Opinion 8.08 - Informed consent. Available at http://www.ama-assn.org/
- Elsberry RB. The invasion of the body scanners. Imaging Economics, Feb 2002. Available at http://www.imagingeconomics.com/
- American College of Radiology. ACR statement on whole-body CT screening. Sep 2002. Available at http://www.acr.org/
- Greenland P, Bonow RO, Brundage BH, et al. ACCF/AHA 2007 clinical expert consensus document on coronary artery calcium scoring by computed tomography in global cardiovascular risk assessment and in evaluation of patients with chest pain: a report of the American College of Cardiology Foundation Clinical Expert Consensus Task Force. J Am Coll Cardiol 2007; 49:378-402.
- National Cancer Institute National Lung Screening Trial. Available at http://www.cancer.gov/nlst/
- Levin B, Lieberman DA, McFarland B, et al. Screening and surveillance for the early detection of colorectal cancer and adenomatous polyps, 2008: a joint guideline from the American Cancer Society, the US Multi-Society Task Force on Colorectal Cancer, and the American College of Radiology. Gastroenterology 2008; 134:1570-1595.
- Furtado CD, Aguirre DA, Sirlin CB, et al. Whole-body CT screening: Spectrum of findings and recommendations in 1192 patients. Radiology 2005; 237:385-394.
- Stanley RJ. Inherent dangers in radiologic screening. Am J Roentgenol 2001; 177:989-992.
- Brenner DJ, Elliston CD. Estimated radiation risks potentially associated with full-body CT screening. Radiology 2004; 232:735-738.
- AMA Code of Medical Ethics Opinion 8.045 - Direct-to-consumer diagnostic imaging tests. Available at http://www.ama-assn.org/